
Obesity, respiratory disease and pulmonary infections
Introduction
Body mass index (BMI) is the classification index used by the World Health Organisation (WHO) to define underweight, overweight and obesity in adults. BMI is defined as weight in kilograms divided by the height in metres squared (kg/m2). Adults with a BMI of 18.5–24.9 kg/m2 are classified as normal, 25.0–29.9 kg/m2 as overweight, 30.0–39.9 kg/m2 as obese and ≥40.0 kg/m2 as morbidly obese. Obesity prevalence is increasing in the United Kingdom (UK), from 15% in 1993 to 27% in 2015 (1). In 2015, 58% of women and 68% of men in the UK were overweight or obese, and obesity was recorded as a factor leading to hospital admission in 525,000 cases during 2015–2016 across the country (1).
Obesity in adults is well-known to increase the risk of hypertension, dyslipidemia, diabetes mellitus, coronary artery disease, heart failure, respiratory disease and multiple cancer types. It is considered a non-communicable disease and has a significant impact on patient’s quality of life (QOL) and disability (2). However, the relationship between obesity and infection is less clear and reports on the susceptibility, risks, complications and outcome of infection in obese patients vary across the literature. More recently the concept of “infectobesity” has gained attention, with evidence that infectious agents have a role in the pathogenesis of obesity (3).
Overweight and obesity are associated with an increased risk of all-cause mortality (4) and some authors suggest the stagnation of increasing life expectancy in recent years may be attributable to the increasing prevalence of obesity and its negative effect on longevity (5). Furthermore, as the number of years lived with obesity increases, a dose-dependent increase is also seen in the risk of all-cause, cardiovascular, and cancer mortality (6).
This review aims to describe the complex relationship between adult obesity and the respiratory and immune systems, and the risk and outcome of infections in obese adults with particular focus on respiratory infections. It also aims to highlight the outcomes and morbidity for obese patients in the intensive care unit (ICU) setting and in relation to invasive and non-invasive ventilation (NIV).
The association between obesity and respiratory disease
The most common and well known respiratory disease associated with obesity is obstructive sleep apnoea (OSA). In the UK, approximately 330,000 people are currently diagnosed with OSA (7). However, the British Lung Foundation estimates that 80% of cases of OSA in the UK still remain undiagnosed, increasing the total number of OSA sufferers to 1.5 million (7) and affecting 4% of middle aged men and 2% of middle aged women (8). Well known risk factors for OSA are male gender, increasing age, hypertension, diabetes and obesity. The strongest risk factor is obesity, with OSA prevalence incrementally rising as BMI increases. A prospective cohort study that followed patients up over a 10-year period found a 10% weight gain was associated with a six-fold increase in risk of incident OSA (9). The prevalence of OSA in the UK is expected to rise over coming years due to the increasing prevalence of obesity and the aging UK population. In the United States (US), with a population with a higher average BMI amongst other demographic differences compared to the UK, this translates to a higher estimated OSA prevalence of 15% in men and 5% in women (10-12).
The pathophysiology of OSA is complex. Recurrent upper airway obstruction during sleep causes complete or partial airflow obstruction leading to apnoeas and hypopnoeas respectively. This translates into fragmented sleep with consequent daytime somnolence, poor concentration and tiredness.
Weight loss and non-invasive continuous positive airway pressure (CPAP) ventilation are the mainstay of treatment and OSA must be considered a chronic disease requiring multidisciplinary management. Untreated OSA causes an increased risk of strokes, cardiovascular events including high blood pressure, cardiac arrhythmias, and coronary artery disease, and road traffic accidents and fatalities (13).
Patients with severe obesity, particularly those with a BMI >50 kg/m2, may develop awake alveolar hypoventilation leading to obesity hypoventilation syndrome (OHS). OHS is driven by impaired respiratory mechanics, abnormal central ventilatory control, sleep disordered breathing and metabolic changes (14). Patients present with hypercapnic respiratory failure and the mainstay of treatment is weight loss and non-invasive bilevel positive airway pressure (BiPAP) ventilation. However, a large number of patients have overlap syndromes with OSA and other sleep disordered breathing syndromes requiring a combination of CPAP and BiPAP which must be managed under specialist care. OHS is associated with high morbidity and mortality, especially if left untreated (14).
The third important association between respiratory disease and obesity is the increased risk of venous thromboembolism (VTE) in obese patients. VTE presents as deep vein thromboses or pulmonary emboli (PE). In the UK in 2011 PE’s accounted for 28,000 hospital admissions and 250,000 bed days, and in 2012 2,300 people died of PE, compromising 2% of the total number of people that died from lung diseases that year (15). Virchow’s triad states that a combination of blood flow stasis, endothelial injury and hypercoagulable states result in VTE. Obesity increases the risk of deep vein thromboses and PE, with a significant increase in incidence risk as BMI rises. Some studies report up to a 2.4-fold increased risk of VTE in obese patients compared to those with a normal BMI (16,17). Obesity is a risk factor for recurrent VTE once anticoagulation is stopped, with a population attributable risk of excess body weight of 26.8% (17).
The association between obesity and infection
The link between obesity and infection is becoming increasingly recognised, although the exact mechanisms for this association are still not well established and probably multifactorial. Through the secretion of adipokines, adipose tissue modulates innate and adaptive immune responses independent of microbial infection (3). As well as this immune dysregulation observed in obesity, other confounding issues including medical comorbidities such as chronic kidney disease and type 2 diabetes mellitus, polypharmacy, inappropriate antibiotic dosing and respiratory dysfunction are all likely to play a part in the risk of acquiring infections in obese individuals and the outcome of these once established (18).
The presence of immature haematopoietic cells and bone marrow-derived immune cells in adipose tissue, and the common embryonic origin between adipose and monocyte/macrophage lineages with consequent sharing of expressed and secreted proteins highlight the close association between adipose tissue and the immune system (3). The secretion of immunoregulatory adipokines such as adiponectin and leptin by adipose tissue has a role in the body’s inflammatory response and metabolic landscape (18,19). Adiponectin is the most abundant protein within an adipocyte and has been found have potent immunosuppressive properties through cytokine regulation (20). Low adiponectin levels at admission to the ICU have been identified as an independent predictor of survival (21). Leptin on the other hand has a wide range of effects on the immune system, including activation of polymorphonuclear neutrophils, induction of proliferation of T lymphocytes, affecting cytokine production and regulation of activation of monocytes/macrophages (22). Leptin levels rise sharply during infection and inflammation, and are felt to represent a protective component of the host immune response (23).Genetically modified leptin-deficient ob/ob mice are severely obese, more susceptible to bacterial infections and pneumonia, and exhibit increased sensitivity to proinflammatory stimuli, impaired phagocytic functions and reduced T-cell function (22,23).
Changes in cell signalling, metabolism and thrombogenic responses are other postulated mechanisms for increased risk and severity of infection in obese individuals. Experimental models have found that decreased tumour necrosis factor α (TNF α) production and increased nitric oxide (NO) release, potentially caused by abnormalities in cell signalling or in arginine and glutamine metabolism in macrophages, may contribute to increased susceptibility to infection in obese rats (24). Exaggerated microvascular inflammatory and thrombogenic responses in obese mice contribute to increased morbidity to sepsis compared to their lean counterparts (25). This increased pro-inflammatory and pro-thrombotic risk associated with obesity has also been proven in humans where C-reactive protein (CRP) and fibrinogen levels are strongly related to BMI (26).
From a clinical perspective, a measurable increased risk of infection in obese adults has been reported for a range of infections in a variety of organ systems, although the mechanisms explaining these findings are still uncertain. There is still however limited data, conflicting evidence or no studies for many infections.
Clinically obese individuals present several challenges both in their routine medical and nursing care as well as the diagnosis and management of infection. Poor mobility and inability to perform some/most aspects of self-care, poor skin integrity and increased risk of skin breakdown, difficulty obtaining microbiological samples, issues with the safety and feasibility of diagnostic procedures and invasive testing, multiple comorbidities and limited data regarding antimicrobial dosing in obesity are some of these challenges.
Obese individuals display altered volumes of distribution and changes in metabolism of drugs which may be, in part, due to medical comorbidities like chronic kidney disease and hepatic steatosis. There is little data regarding the correct dosing of antimicrobials in obese patients with studies suggesting these are frequently under-dosed with consequent risks of treatment failure and emergence of antimicrobial resistance (27,28). In obesity it is not clear what the most appropriate drug doses or administration timing is and whether preferential use of lipophilic or hydrophilic drugs is required, and further work is needed in this field (18).
Once established, the outcome of infection in obese individuals seems to be poorer compared to those with normal BMI (29-31). A systematic review found that this poorer outcome from infection was found in both patients at the highest and lowest extremes of BMI, with patients in the lowest BMI group having worse outcome compared to all other groups combined (29).
Respiratory infections in the obese
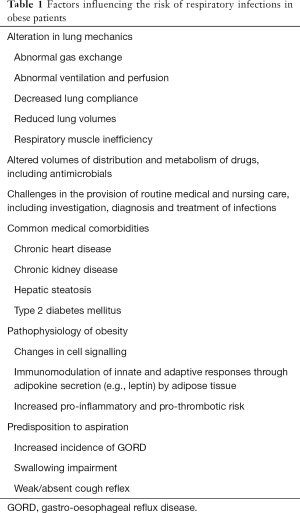
Alteration of lung mechanics in obese patients including reduced lung volumes, decreased compliance, abnormal ventilation and perfusion relationship and gas exchange, and respiratory muscle inefficiency can predispose to increased risk and severity of respiratory infections (32). Table 1 outlines the main factors influencing the risk of respiratory infections in the obese. The main areas of evidence around the risk of pulmonary infections in the obese is in community acquired pneumonia (CAP) and flu pneumonitis with equipoise regarding the magnitude of increased risk in both infections.
Full table
About half of patients with OSA have swallowing impairment that predisposes them to aspiration (33). Patients with OSA may also be affected by a weak or absent cough reflex mainly during rapid eye movement (REM) sleep and commonly suffer with gastro-oesophageal reflux disease (GORD) (34). All these factors are postulated to potentially increase their risk of CAP. Studies have shown OSA and OSA severity are associated with CAP (34) and that OSA is an independent risk factor for higher rates of mechanical ventilation, increased risk of clinical deterioration and higher resource use in patients with pneumonia (35). As well as the well-known risk factors for pneumonia including smoking, aging and immunocompromise, BMI is directly associated with the risk of CAP in women (36) and risk of hospitalisation with CAP in men (37). Excessive weight gain over a 2-year follow up (≥18 kg) increases the risk of CAP two-fold in both men and women (36). However, in the field of pneumonia equipoise regarding the effect of obesity on the outcome of infection exists, with some studies indicating that in hospitalised patients with pneumonia OSA is associated with decreased in-hospital mortality in both non-ventilated (35,38) and mechanically-ventilated patients (39). Obesity was also found to not be associated with length of stay (LOS) or transfer to ICU in patients with pneumonia in a retrospective analysis of 717 consecutive patients (38). These conflicting results may be explained by differences in the definitions used for diagnosis of CAP, variations in study adjustments for comorbidities and demographic factors, and disparity in calculations of weight and BMI across studies.
The evidence of the effect of obesity on the risk and severity of flu pneumonitis is mainly based on the influenza A H1N1 pandemic of 2009. The difficulties in obtaining information regarding risk and outcome of flu pneumonitis is down to the challenge of using various case-definitions, case-ascertainment and availability of diagnostic testing. The gold standard case-definition of a confirmed case of H1N1 is one that is laboratory-confirmed, but this only represents a small number of the total symptomatic cases and these in turn are only a fraction of the total seroincidence of a viral infection across a population. WHO reported 18,500 deaths worldwide of laboratory-confirmed H1N1 during the pandemic, however modelling studies suggest this is a gross underestimate with the total global number predicted to be 201,200 respiratory deaths and 83,300 cardiovascular deaths secondary to H1N1 (40). In the UK using the definition for a fatal H1N1 case to be an H1N1 laboratory-confirmed death or one where H1N1 was recorded in the death certificate, 440 deaths due to H1N1 were reported up to March 2012 with an overall symptomatic case fatality ratio (CFR) of 0.4 per 1,000 clinical cases [95% confidence interval (CI): 0.2–1.0] (41). This CFR rose to 0.9 per 1,000 clinical cases in pregnant women, 9 per 1,000 clinical cases in those over 65 years of age, and 14 per 1,000 clinical cases in patients >65 years with at least one risk factor (chronic respiratory disease, chronic heart disease, chronic liver disease, chronic renal disease, chronic neurological disease, stroke/transient ischaemic attack, immunosuppression and diabetes) (41).
A global pooled analysis undertaken by the WHO of 70,000 laboratory-confirmed hospitalised H1N1 patients showed the proportion of patients with obesity increased with rising H1N1 disease severity, with a pooled odds ratio (OR) for death of 2.9 (95% CI: 1.3–6.6) in obese patients (42). A meta-analysis of 6 cross-sectional studies including hospitalised patients with H1N1 also reported obesity to be associated with higher risks of ICU admission and death (43). This association between obesity and severe outcomes from H1N1 is postulated to be due to direct causation (e.g., greater respiratory strain of infection on obese individuals), causation through other known risk factors (e.g., obesity causes diabetes and heart disease, which also pose an increased risk for severe outcome of H1N1), or a non-causal association (42). Subsequent studies in France, Spain, the US, and Canada have replicated these findings and have shown obesity is associated with increased hospitalisation, ICU admission and fatal outcome from H1N1 (44-47). However, studies in developing countries, where the majority of the world’s population live and the bulk of H1N1 infection was believed to occur are lacking.
The increased risk of adverse outcomes in obesity during the 2009 H1N1 pandemic had not previously been recognised as a risk factor during seasonal influenza epidemics. However, a cohort study spanning 12 influenza seasons in Canada showed morbidly obese individuals with or without other known risk factors are at increased risk of respiratory hospitalisations during influenza seasons (48). In 2014 the Joint Committee on Vaccination and Immunisation (JCVI) in the UK advised patients with morbid obesity should be offered seasonal influenza vaccination as part of the national immunisation programme. However, the response to Influenza vaccination may be affected by obesity, with one study reporting increasing BMI being associated with greater declines in influenza-specific antibody titres after 1 year and influenza-stimulated T-cells in the obese being less functional compared to those in healthy weight adults (19).
Given the difficulties in case-ascertainment of H1N1 and the lack of data regarding patient’s BMI in non-hospitalised patients it has been difficult to date to establish a differential risk both in susceptibility to influenza infection in obese patients and the outcome of infection in obese patients with disease not requiring hospitalisation.
Despite widespread use of oseltamivir during the 2009 H1N1 pandemic and continuing use during seasonal epidemics its efficacy for the treatment of Influenza is still widely debated. Pharmacokinetic data shows that oseltamivir does not need to be dose-adjusted for body weight in morbidly obese individuals in single or multiple dosing regimens (49). However, the debate regarding the value of oseltamivir is set to continue with its recent downgrade from a “core” to a “complementary” drug in the WHO’s list of essential medicines (50).
Impact of obesity on infection risk in the ICU setting
Focusing particularly in the ICU setting, the impact of obesity on the risk of acquiring infections, morbidity and outcome in the intensive care setting has been widely published. However, there is debate regarding the effect of obesity on various outcomes, with studies occasionally publishing conflicting results. One of the factors influencing this diversity in study findings is the heterogeneity in the patient population requiring ICU admission with many publications only studying population subgroups such as surgical patients, trauma cases and patients with septic shock, which does not allow the generalisation of study findings to the wider patient population. Another challenge is the difficulty in obtaining accurate BMI data on critically ill patients with some studies using estimated body weights instead. Recorded weights may also not be a true reflection of the patient’s actual weight because of vascular fluid volume depletion (18). There is also heterogeneity in study outcomes between overweight, obese and morbidly obese patients indicating they are not one homogeneous patient cohort. The challenges of antimicrobial prescribing are still very pertinent in the ICU setting, with frequent under and overdosing of antibiotics in obese patients and appropriate therapeutic drug monitoring (TDM) levels being less frequently achieved (51).
Numerous retrospective and prospective studies have shown an increased risk of infections in obese surgical and trauma patients, those admitted with septic shock and in unselected patient cohorts in the ICU setting (52-57). Bloodstream infections are more prevalent in older obese patients regardless of the hospital setting (58). This increased risk of blood stream infections has also been shown in the ICU setting in morbidly obese post-operative patients (55), obese trauma patients (56) and morbidly obese unselected patient cohorts (54). Other infections associated with obesity in the ICU have been catheter related infections (52,54,55), respiratory infections (53,54,56), urinary tract infections (UTI) (56) and wound infections (53). A large prospective multicentre study of 2,878 unselected patients requiring ICU admission in 198 European study centres across 24 countries found obese and morbidly obese patients were significantly more likely to develop an ICU-acquired infection compared to those with normal BMI’s although there was no difference in the incidence of sepsis syndromes across different BMI groups (57).
More research is needed in the risk and outcomes of obese patients requiring ICU admission as despite their increased risk of infections, theoretical problems with mechanical ventilation and increased risk of other complications, the effect on morbidity and mortality is still undetermined. Study design heterogeneity, difference in patient populations and difference in reporting outcomes has been a challenge that has hindered generalisability and comparison of studies.
Morbidity in OSA management
With the increasing use of both acute and long-term ventilation devices in obese patients the incidence and range of complications associated with these has become increasingly recognised. The effect of these complications on obese patients is especially pertinent due to the inherent challenges they pose when mechanically ventilated in the ICU setting but also as they are some of the most frequent users of NIV devices (CPAP or BiPAP).
Ventilator-associated pneumonia (VAP) is the most important complication of mechanical ventilation and carries with it significant morbidity, mortality and cost (59,60). VAP is often described as nosocomial pneumonia within ≥48 h of intubation with an endotracheal or tracheostomy tube. However, diagnosis is challenging as it mainly relies on clinical criteria alone (61) with three or more of the following usually being required: fever, leucocytosis/leucopenia, purulent secretions and a new and/or persistent infiltrate on chest X-ray (60). Up to a quarter of patients receiving mechanical ventilation will suffer VAP with a consequent 24–50% mortality rate (62). Research suggests patients with VAP have significantly longer ICU LOS and incur up to $10,019 in additional hospital costs (59).
The risk of pneumonia in patients receiving NIV is less well defined and is most certainly lower than patients with endotracheal ventilation although their use of a respirator and ventilator circuit does theoretically put them at increased risk compared to non-ventilated patients (63). Other NIV-specific complications can also occur, with reported rates of complications varying between 30% and 50% (64). These complications can negatively impact on the patient’s tolerance and the efficacy of NIV, potentially leading to NIV failure. Nasal bridge ulceration mainly due to over-tightening, skin reactions secondary to latex allergy, severe gastric distension, sinus or ear discomfort, nasal mucosal congestion or drying/ulceration can all be common and should be addressed to maximise patient compliance and efficacy of NIV. The use of humidifiers to prevent some of these side-effects is of uncertain benefit (64). There is some evidence that NIV-associated upper airway infections are a complication of NIV use, and in patients using humidifiers it is hypothesized this may be caused by microbial contamination of the humidifier in part due to poor maintenance of these component parts (65). An acute pneumothorax is a life-threatening complication of NIV therapy that should be actively excluded in all patients who develop unexplained agitation/distress of chest pain (64).
Conclusions
Obesity is becoming an increasingly prevalent and problematic comorbidity in patients with wide-ranging resource and cost implications across health care systems. There is an expanding body of evidence that reflects this and attempts to draw conclusions regarding the effect of obesity on the pathophysiology and management of respiratory disease, the risk of susceptibility to and outcome from infection, and hospital and ICU morbidity and mortality.
Obesity has a direct causal effect on some respiratory diseases, namely OSA and OHS. It is also strongly associated with some infections, although it’s relative effect varies across infection types and organ systems. The influenza A H1N1 pandemic of 2009 focused researcher’s attention on the interaction between obesity and respiratory infections, namely flu pneumonitis, but further research is needed in this field and in other respiratory infections. Management of infectious complications associated with treatment of OSA and OHS and management of obese patients in the ICU requires further work to establish the effect of obesity on outcome and morbidity.
The exact mechanisms underpinning all these complex interactions are still not entirely understood and require more research. All these mentioned associations are probably multifactorial and large prospective studies are required to try to understand the relative importance of obesity, comorbid conditions and challenges in management of such patients.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- NHS Digital. Statistics on Obesity, Physical Activity and Diet. Available online: https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/613532/obes-phys-acti-diet-eng-2017-rep.pdf
- Sirtori A, Brunani A, Villa V, et al. Obesity is a marker of reduction in QoL and disability. ScientificWorldJournal 2012;2012:167520.
- Hegde V, Dhurandhar NV. Microbes and obesity--interrelationship between infection, adipose tissue and the immune system. Clin Microbiol Infect 2013;19:314-20. [Crossref] [PubMed]
- Aune D, Sen A, Prasad M, et al. BMI and all cause mortality: systematic review and non-linear dose-response meta-analysis of 230 cohort studies with 3.74 million deaths among 30.3 million participants. BMJ 2016;353:i2156. [Crossref] [PubMed]
- Olshansky SJ, Passaro DJ, Hershow RC, et al. A potential decline in life expectancy in the United States in the 21st century. N Engl J Med 2005;352:1138-45. [Crossref] [PubMed]
- Abdullah A, Wolfe R, Stoelwinder JU, et al. The number of years lived with obesity and the risk of all-cause and cause-specific mortality. Int J Epidemiol 2011;40:985-96. [Crossref] [PubMed]
- Rejon-Parrilla JC, Garau M, Sussex J. Obstructive Sleep Apnoea: Health Economics Report. Office of Health Economics 2014. Available online: https://www.ohe.org/publications/obstructive-sleep-apnoea-health-economics-report#
- Steier J, Martin A, Harris J, et al. Predicted relative prevalence estimates for obstructive sleep apnoea and the associated healthcare provision across the UK. Thorax 2014;69:390-2. [Crossref] [PubMed]
- Peppard PE, Young T, Palta M, et al. Longitudinal study of moderate weight change and sleep-disordered breathing. JAMA 2000;284:3015-21. [Crossref] [PubMed]
- Young T, Palta M, Dempsey J, et al. Burden of sleep apnea: rationale, design, and major findings of the Wisconsin Sleep Cohort study. WMJ 2009;108:246-9. [PubMed]
- Peppard PE, Young T, Barnet JH, et al. Increased prevalence of sleep-disordered breathing in adults. Am J Epidemiol 2013;177:1006-14. [Crossref] [PubMed]
- Dempsey JA, Veasey SC, Morgan BJ, et al. Pathophysiology of sleep apnea. Physiol Rev 2010;90:47-112. [Crossref] [PubMed]
- Harding SM. Complications and consequences of obstructive sleep apnea. Curr Opin Pulm Med 2000;6:485-9. [Crossref] [PubMed]
- Marik PE, Desai H. Characteristics of patients with the "malignant obesity hypoventilation syndrome" admitted to an ICU. J Intensive Care Med 2013;28:124-30. [Crossref] [PubMed]
- British Lung Foundation. Pulmonary embolism statistics. Available online: https://statistics.blf.org.uk/pulmonary-embolism
- Tsai AW, Cushman M, Rosamond WD, et al. Cardiovascular risk factors and venous thromboembolism incidence: the longitudinal investigation of thromboembolism etiology. Arch Intern Med 2002;162:1182-9. [Crossref] [PubMed]
- Pomp ER, le Cessie S, Rosendaal FR, et al. Risk of venous thrombosis: obesity and its joint effect with oral contraceptive use and prothrombotic mutations. Br J Haematol 2007;139:289-96. [Crossref] [PubMed]
- Huttunen R, Syrjänen J. Obesity and the risk and outcome of infection. Int J Obes (Lond) 2013;37:333-40. [Crossref] [PubMed]
- Green WD, Beck MA. Obesity altered T cell metabolism and the response to infection. Curr Opin Immunol 2017;46:1-7. [Crossref] [PubMed]
- Wolf AM, Wolf D, Rumpold H, et al. Adiponectin induces the anti-inflammatory cytokines IL-10 and IL-1RA in human leukocytes. Biochem Biophys Res Commun 2004;323:630-5. [Crossref] [PubMed]
- Koch A, Sanson E, Voigt S, et al. Serum adiponectin upon admission to the intensive care unit may predict mortality in critically ill patients. J Crit Care 2011;26:166-74. [Crossref] [PubMed]
- Falagas ME, Kompoti M. Obesity and infection. Lancet Infect Dis 2006;6:438-46. [Crossref] [PubMed]
- Faggioni R, Feingold KR, Grunfeld C. Leptin regulation of the immune response and the immunodeficiency of malnutrition. FASEB J 2001;15:2565-71. [Crossref] [PubMed]
- Blanc MC, Moinard C, Beziel A, et al. Arginine and glutamine availability and macrophage functions in the obese insulin-resistant Zucker rat. J Cell Physiol 2005;202:153-9. [Crossref] [PubMed]
- Vachharajani V, Russell JM, Scott KL, et al. Obesity exacerbates sepsis-induced inflammation and microvascular dysfunction in mouse brain. Microcirculation 2005;12:183-94. [Crossref] [PubMed]
- Festa A, D'Agostino R Jr, Williams K, et al. The relation of body fat mass and distribution to markers of chronic inflammation. Int J Obes Relat Metab Disord 2001;25:1407-15. [Crossref] [PubMed]
- Roe JL, Fuentes JM, Mullins ME. Underdosing of common antibiotics for obese patients in the ED. Am J Emerg Med 2012;30:1212-4. [Crossref] [PubMed]
- Falagas ME, Karageorgopoulos DE. Adjustment of dosing of antimicrobial agents for bodyweight in adults. Lancet 2010;375:248-51. [Crossref] [PubMed]
- Falagas ME, Athanasoulia AP, Peppas G, et al. Effect of body mass index on the outcome of infections: a systematic review. Obes Rev 2009;10:280-9. [Crossref] [PubMed]
- Lizza BD, Rhodes NJ, Esterly JS, et al. Impact of body mass index on clinical outcomes in patients with gram-negative bacteria bloodstream infections. J Infect Chemother 2016;22:671-6. [Crossref] [PubMed]
- Paulsen J, Askim A, Mohus RM, et al. Associations of obesity and lifestyle with the risk and mortality of bloodstream infection in a general population: a 15-year follow-up of 64 027 individuals in the HUNT Study. Int J Epidemiol 2017. [Epub ahead of print]. [Crossref] [PubMed]
- Ashburn DD, DeAntonio A, Reed MJ. Pulmonary system and obesity. Crit Care Clin 2010;26:597-602. [Crossref] [PubMed]
- Schindler A, Mozzanica F, Sonzini G, et al. Oropharyngeal Dysphagia in patients with obstructive sleep apnea syndrome. Dysphagia 2014;29:44-51. [Crossref] [PubMed]
- Chiner E, Llombart M, Valls J, et al. Association between Obstructive Sleep Apnea and Community-Acquired Pneumonia. PloS One 2016;11:e0152749. [Crossref] [PubMed]
- Lindenauer PK, Stefan MS, Johnson KG, et al. Prevalence, treatment, and outcomes associated with OSA among patients hospitalized with pneumonia. Chest 2014;145:1032-8. [Crossref] [PubMed]
- Baik I, Curhan GC, Rimm EB, et al. A prospective study of age and lifestyle factors in relation to community-acquired pneumonia in US men and women. Arch Intern Med 2000;160:3082-8. [Crossref] [PubMed]
- Kornum JB, Norgaard M, Dethlefsen C, et al. Obesity and risk of subsequent hospitalisation with pneumonia. Eur Respir J 2010;36:1330-6. [Crossref] [PubMed]
- Atamna A, Elis A, Gilady E, et al. How obesity impacts outcomes of infectious diseases. Eur J Clin Microbiol Infect Dis 2017;36:585-91. [Crossref] [PubMed]
- Jean RE, Gibson CD, Jean RA, et al. Obstructive sleep apnea and acute respiratory failure: An analysis of mortality risk in patients with pneumonia requiring invasive mechanical ventilation. J Crit Care 2015;30:778-83. [Crossref] [PubMed]
- Dawood FS, Iuliano AD, Reed C, et al. Estimated global mortality associated with the first 12 months of 2009 pandemic influenza A H1N1 virus circulation: a modelling study. Lancet Infect Dis 2012;12:687-95. [Crossref] [PubMed]
- Pebody RG, McLean E, Zhao H, et al. Pandemic Influenza A (H1N1) 2009 and mortality in the United Kingdom: risk factors for death, April 2009 to March 2010. Euro Surveill 2010;15. [PubMed]
- Van Kerkhove MD, Vandemaele KA, Shinde V, et al. Risk factors for severe outcomes following 2009 influenza A (H1N1) infection: a global pooled analysis. PLoS Med 2011;8:e1001053. [Crossref] [PubMed]
- Fezeu L, Julia C, Henegar A, et al. Obesity is associated with higher risk of intensive care unit admission and death in influenza A (H1N1) patients: a systematic review and meta-analysis. Obes Rev 2011;12:653-9. [Crossref] [PubMed]
- Fuhrman C, Bonmarin I, Paty AC, et al. Severe hospitalised 2009 pandemic influenza A(H1N1) cases in France, 1 July-15 November 2009. Euro Surveill 2010;15. [PubMed]
- Kumar A, Zarychanski R, Pinto R, et al. Critically ill patients with 2009 influenza A(H1N1) infection in Canada. JAMA 2009;302:1872-9. [Crossref] [PubMed]
- Rello J, Rodriguez A, Ibanez P, et al. Intensive care adult patients with severe respiratory failure caused by Influenza A (H1N1)v in Spain. Crit Care 2009;13:R148. [Crossref] [PubMed]
- Morgan OW, Bramley A, Fowlkes A, et al. Morbid obesity as a risk factor for hospitalization and death due to 2009 pandemic influenza A(H1N1) disease. PloS One 2010;5:e9694. [Crossref] [PubMed]
- Kwong JC, Campitelli MA, Rosella LC. Obesity and respiratory hospitalizations during influenza seasons in Ontario, Canada: a cohort study. Clin Infect Dis 2011;53:413-21. [Crossref] [PubMed]
- Thorne-Humphrey LM, Goralski KB, Slayter KL, et al. Oseltamivir pharmacokinetics in morbid obesity (OPTIMO trial). J Antimicrob Chemother 2011;66:2083-91. [Crossref] [PubMed]
- Kmietowicz Z. WHO downgrades oseltamivir on drugs list after reviewing evidence. BMJ 2017;357:j2841. [Crossref] [PubMed]
- Tafelski S, Yi H, Ismaeel F, et al. Obesity in critically ill patients is associated with increased need of mechanical ventilation but not with mortality. J Infect Public Health 2016;9:577-85. [Crossref] [PubMed]
- Wurzinger B, Dunser MW, Wohlmuth C, et al. The association between body-mass index and patient outcome in septic shock: a retrospective cohort study. Wien Klin Wochenschr 2010;122:31-6. [Crossref] [PubMed]
- Serrano PE, Khuder SA, Fath JJ. Obesity as a risk factor for nosocomial infections in trauma patients. J Am Coll Surg 2010;211:61-7. [Crossref] [PubMed]
- Yaegashi M, Jean R, Zuriqat M, et al. Outcome of morbid obesity in the intensive care unit. J Intensive Care Med 2005;20:147-54. [Crossref] [PubMed]
- Dossett LA, Dageforde LA, Swenson BR, et al. Obesity and site-specific nosocomial infection risk in the intensive care unit. Surg Infect (Larchmt) 2009;10:137-42. [Crossref] [PubMed]
- Bochicchio GV, Joshi M, Bochicchio K, et al. Impact of obesity in the critically ill trauma patient: a prospective study. J Am Coll Surg 2006;203:533-8. [Crossref] [PubMed]
- Sakr Y, Madl C, Filipescu D, et al. Obesity is associated with increased morbidity but not mortality in critically ill patients. Intensive Care Med 2008;34:1999-2009. [Crossref] [PubMed]
- Kaye KS, Marchaim D, Chen TY, et al. Predictors of nosocomial bloodstream infections in older adults. J Am Geriatr Soc 2011;59:622-7. [Crossref] [PubMed]
- Safdar N, Dezfulian C, Collard HR, et al. Clinical and economic consequences of ventilator-associated pneumonia: a systematic review. Crit Care Med 2005;33:2184-93. [Crossref] [PubMed]
- Masterton RG, Galloway A, French G, et al. Guidelines for the management of hospital-acquired pneumonia in the UK: report of the working party on hospital-acquired pneumonia of the British Society for Antimicrobial Chemotherapy. J Antimicrob Chemother 2008;62:5-34. [Crossref] [PubMed]
- Kalil AC, Metersky ML, Klompas M, et al. Management of Adults With Hospital-acquired and Ventilator-associated Pneumonia: 2016 Clinical Practice Guidelines by the Infectious Diseases Society of America and the American Thoracic Society. Clin Infect Dis 2016;63:e61-111. [Crossref] [PubMed]
- Chastre J, Fagon JY. Ventilator-associated pneumonia. Am J Respir Crit Care Med 2002;165:867-903. [Crossref] [PubMed]
- Benhamou D, Cuvelier A, Muir JF. Prevention of infections transmitted by CPAP and noninvasive ventilation. Rev Pneumol Clin 2001;57:73-8. [PubMed]
- Davidson AC, Banham S, Elliott M, et al. BTS/ICS guideline for the ventilatory management of acute hypercapnic respiratory failure in adults. Thorax 2016;71 Suppl 2:ii1-35. [Crossref] [PubMed]
- Sanner BM, Fluerenbrock N, Kleiber-Imbeck A, et al. Effect of continuous positive airway pressure therapy on infectious complications in patients with obstructive sleep apnea syndrome. Respiration 2001;68:483-7. [Crossref] [PubMed]
Cite this article as: Fernandez C, Manuel A. Obesity, respiratory disease and pulmonary infections. Ann Res Hosp 2017;1:38.


